Introduction
Migraines are more than just headaches—they are a debilitating neurological condition that can affect daily life, productivity, sleep, and overall well-being. While medications help manage symptoms, research shows that physiotherapy offers long-term, non-invasive, and evidence-based relief by targeting the root physical triggers of migraine attacks.
If you experience neck pain, posture issues, stress, or muscle tension, physiotherapy may significantly reduce both the frequency and severity of your migraines.
What Causes Migraines?
Migraines can be triggered by:
Muscle tension in the neck and upper back
Cervical spine dysfunction
Poor posture
Jaw (TMJ) dysfunction
Stress and lack of sleep
Hormonal fluctuations
Eye strain from screens
Physical overuse or inactivity
Many of these factors are musculoskeletal, which is why physiotherapy plays an essential role in migraine management.
How Physiotherapy Helps with Migraines
Multiple studies show that physiotherapy can:
Reduce intensity of migraine episodes
Decrease frequency of attacks
Improve neck mobility and posture
Lower muscle tension
Enhance relaxation and stress management
Reduce reliance on pain medications
Physiotherapists use a combination of manual therapy, posture retraining, exercises, and lifestyle correction to address root causes.
1. Manual Therapy for Migraine Relief
Manual therapy techniques supported by research include:
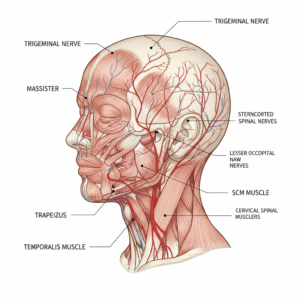
• Cervical Spine Mobilization
Improves neck mobility and reduces stiffness that triggers migraines.
• Soft Tissue Release
Targets tight muscles in the neck, shoulders, and upper back.
• Trigger Point Therapy
Relieves knots in the upper trapezius, levator scapulae, suboccipitals—common migraine-driving muscles.
• TMJ Therapy
For patients with jaw pain or teeth grinding (a major migraine contributor).
2. Posture Correction & Ergonomics
Poor posture—especially forward head posture from long screen time—is a major cause of migraines.
Physiotherapy helps by:
Teaching neutral spine alignment
Improving ergonomic setup for desk work
Strengthening postural muscles
Reducing upper cervical strain
Correct posture reduces strain on the suboccipital region, where many migraine nerves originate.
3. Strengthening & Stretching Exercises
Evidence-based exercises include:
Neck Strengthening
Deep neck flexor activation
Scapular stabilizing exercises
Flexibility & Stretching
Upper trapezius stretch
Levator scapulae stretch
Suboccipital release
Pectoral stretching
Relaxation Exercises
Diaphragmatic breathing
Gentle yoga-based neck stretches
Doing these regularly reduces muscle tension and prevents migraine episodes.
4. Vestibular Physiotherapy (If Dizziness Is Present)
Some migraines involve dizziness or visual disturbances. Vestibular therapy helps with:
Balance training
Eye-head coordination
Motion sensitivity
Dizziness reduction
This improves daily functioning and reduces migraine triggers.
5. Lifestyle & Self-Management Strategies
Your physiotherapist may also guide you on:
✔ Sleep hygiene
✔ Hydration
✔ Activity pacing
✔ Screen-time breaks
✔ Stress-reduction techniques
These changes support long-term migraine control.
When to See a Physiotherapist?
You should consult a physiotherapist if:
Your migraines are triggered by neck pain
You experience frequent headaches during desk work
Stress increases your symptoms
You have stiffness in the upper back or jaw
Medication alone is not working
Physiotherapy provides a drug-free, clinically proven approach to managing chronic migraines.
Conclusion
Physiotherapy is a powerful, evidence-based method to manage migraines by targeting the musculoskeletal and lifestyle factors that trigger attacks. Whether through manual therapy, posture correction, strengthening exercises, or ergonomic guidance, physiotherapy offers long-term relief and improved quality of life.
If migraines are limiting your daily routine, physiotherapy can help you feel better and live pain-free.

